(604 words)
Do you devour the vast choice of dental titles that arrive in your practice each month, or only flick through them? Either way, you’ll spot a recurring topic across dental academic and frontline treatment areas: biofilm.
Biofilm is an ever-present risk that impacts the entire spectrum of oral health, with its most common manifestation being plaque. Indeed, one of the largest toothpaste manufacturers refers to it extensively in their current campaigns. But biofilm is omnipresent across most other significant areas of reactive dental treatment, increasing infection risks in peri-implantitis, periodontitis, and endodontic disease in the oral cavity. Once you get into the wider dental practice environment, it can be found on instruments, worktops, devices, equipment and furniture. As well as inside waterlines. So it is pretty much central to every facet of dental treatment.
As with all risk mitigation, understanding what biofilm is and how it forms is a vital first step in taking control of the situation. Armed with this knowledge, dental professionals can provide satisfactory solutions – through education to change in-practice behaviours and with the intervention of professional treatment and products.
So, what is biofilm and how does it form?
Clustering microorganisms can rapidly and unexpectedly form biofilm colonies. Its formation is like the 80s Martini tagline: anytime, anyplace, anywhere! Yet some Infection Control companies claim that their products make biofilm unlikely to form. One water purification system claims that its use means biofilm will never form.
When dental infection control suppliers fail to proactively address biofilm formation- you have to ask why?. Biofilm ‘blind spots’ often stem from a lack of understanding about how biofilm form and not knowing how to resolve them. Or they might not have a product that can eliminate it quickly and safely (non-cytotoxic). Sound scientific knowledge of microbiology proves that biofilm is highly unpredictable. You need to take proactive steps to optimise treatment outcomes. If you understand the five stages of biofilm formation, you can quickly and easily mitigate it.
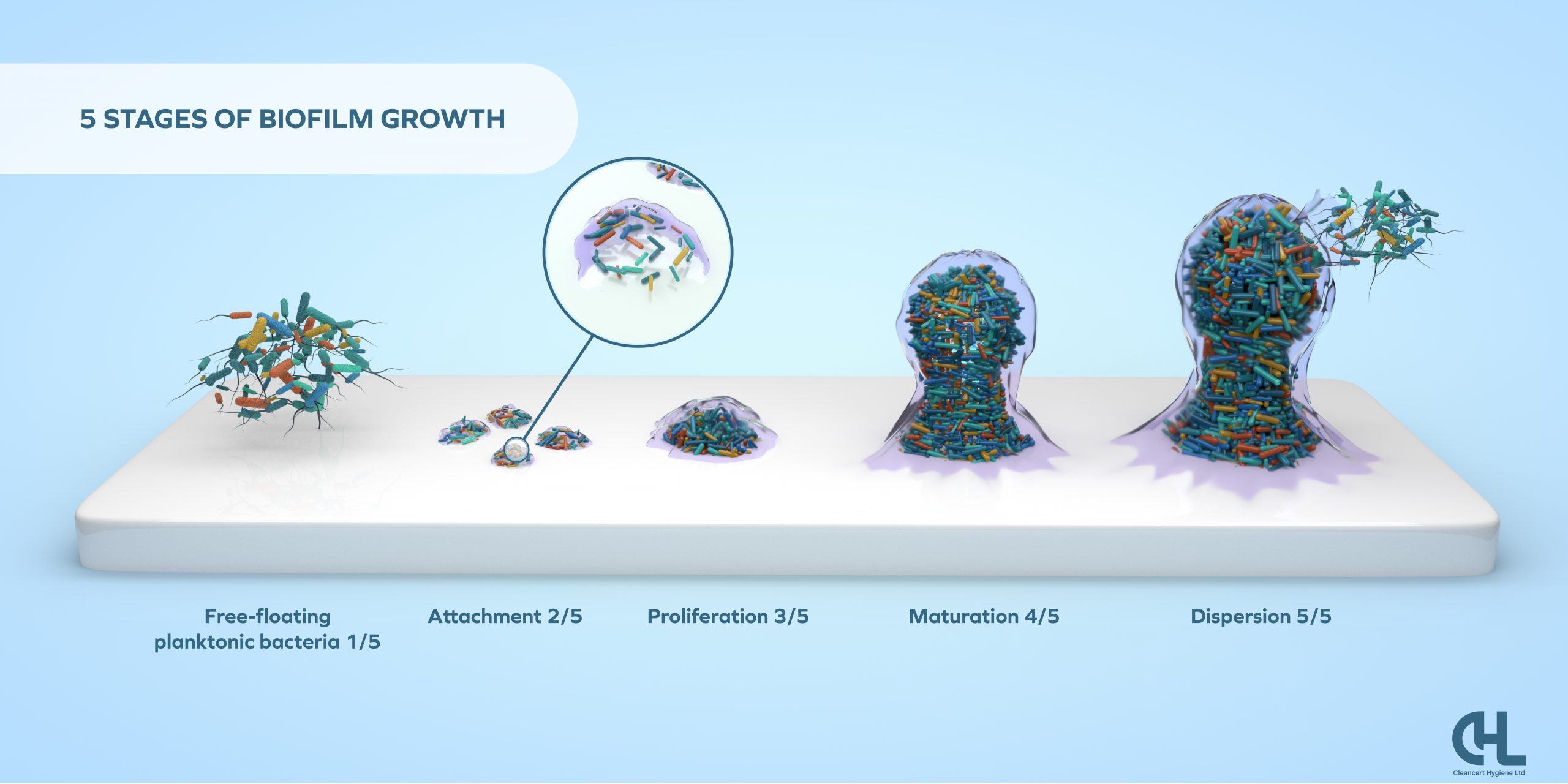
Most infection control products focus their attention on Stage 1. This is because eliminating free floating planktonic bacteria is relatively straightforward, using actives such as alcohols, quaternary ammonium compounds (QACs), chlorine-based strong acids like hypochlorite, and weaker acids like hypochlorous.
Harder-to-tackle problems arise when bacteria attach to surfaces (teeth, gums, implants, wet surfaces) or accumulate in pockets in the roots of teeth. Then the extraordinarily fast and efficient natural process of biofilm formation occurs. Scientists are still trying to fully understand this natural phenomenon. But beyond doubt is that if left unchecked, biofilm can be harmful – even fatal – to dental patients.
The added problem for everyday dentistry is that the only way to assess biofilm growth is by using large and expensive scanning electron microscopes (SEM). This is well beyond the reasonable expectations of a dental professional to measure. Hence there is a need to focus on awareness and proactive mitigation measures.


Balancing up the risks against the effort and cost of finding a solution is something dental professionals do every day. Traditional biofilm treatments have required a combination of mechanical interventions, abrasive scraping, and often cytotoxic chemicals to penetrate the slimy, protective extracellular matrix. We know that these processes can feel onerous for general dental treatment by practice principals, but there are fast, safe (non-cytotoxic) and effective solutions.
Speedy, safe, and proactive solutions for tackling biofilm
CHL’s products have been independently and repeatedly proven to be highly effective against dental biofilms. OraWize+ tackles oral manifestations in endodontics and periodontitis, OptiZil treats surfaces and skin, and CleanCert treats waterlines – all with short contact times and extraordinary non-toxic safety profiles. Do you want to find out how the CHL product range can proactively and reactively optimise your dental treatment outcomes?
Simon Davies is founder and Commercial Director of Tec Safe, a dental company that specialises in developing easier and safer decontamination products for a wide variety of dental applications, using eco-friendly solutions.
Visit the website: www.tec-safe.com
For further info, please email: sales@cleancert-hygiene.co.uk