
(1426 words)
‘Sustainable Dentistry’ is now embedded as one of the key recurring themes across all dental practices – but what does that mean for dental professionals in their everyday work? In this article, Simon Davies, founder of CleanCert Hygiene, continues his Green Dentistry series, focusing on an aspect of the sector that has traditionally used highly corrosive chemicals.
Biofilms – the sticky, slimy build-up of bacteria on surfaces like your teeth – represent a very real hazard in the dental environment. Biofilms are the reason for most frontline dental treatment, from plaque to endodontic to periodontal to peri-implantitis disease.
But biofilms are also a problem in the wider dental practice environment, present on instruments, worktops, devices, equipment and furniture. They can infiltrate dental unit waterlines (DUWLs) and can be found lurking in the water as Legionellosis, an umbrella term for several diseases caused by legionella bacteria.
Biofilms are becoming increasingly problematic in dentistry, with studies[i] suggesting most infections – particularly those considered chronic and worsening – are down to biofilm formation. Dental plaque is a prime example of a biofilm. Regularly removing it is key to preventing and treating caries and periodontal diseases, which are considered the most common diseases of mankind[ii], thanks to Western diets high in sugar and saturated fats.
If left untreated, with antibiotics or antimicrobial agents, biofilm infections can worsen and require teeth, implants or prostheses to be removed. Research suggests this is a growing problem because dentistry is using increasing amounts of plastics and implantable materials that play host to biofilm growth. Oral diseases linked to biofilms are also risk factors for other diseases such as cancer and cardiovascular disease.[iii]
To alleviate the risks posed by biofilms, dental professionals must understand what they are, how they form, and how to eliminate them through changes in in-practice behaviours and procedures.
But biofilms are also a problem in the wider dental practice environment, present on instruments, worktops, devices, equipment and furniture. They can infiltrate dental unit waterlines (DUWLs) and can be found lurking in the water as Legionellosis, an umbrella term for several diseases caused by legionella bacteria.
Biofilms are becoming increasingly problematic in dentistry, with studies[i] suggesting most infections – particularly those considered chronic and worsening – are down to biofilm formation. Dental plaque is a prime example of a biofilm. Regularly removing it is key to preventing and treating caries and periodontal diseases, which are considered the most common diseases of mankind[ii], thanks to Western diets high in sugar and saturated fats.
If left untreated, with antibiotics or antimicrobial agents, biofilm infections can worsen and require teeth, implants or prostheses to be removed. Research suggests this is a growing problem because dentistry is using increasing amounts of plastics and implantable materials that play host to biofilm growth. Oral diseases linked to biofilms are also risk factors for other diseases such as cancer and cardiovascular disease.[iii]
To alleviate the risks posed by biofilms, dental professionals must understand what they are, how they form, and how to eliminate them through changes in in-practice behaviours and procedures.
The problem with biofilm
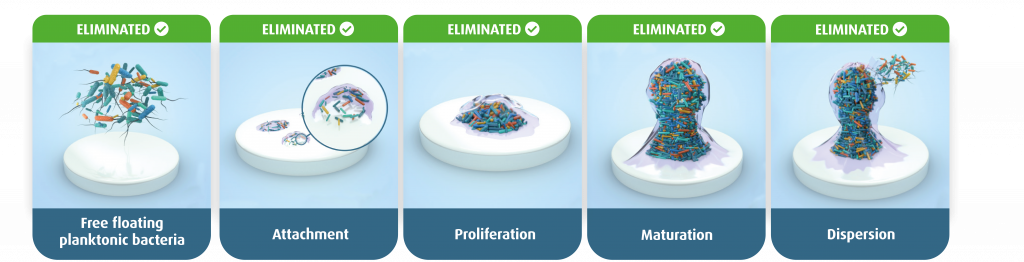
Biofilms are essentially sticky, slimy coatings found on wet surfaces; they consist of bacteria, fungi or protists that clump together and colonise damp or submerged surfaces. They go through five stages of growth. Firstly, groups of free-floating microorganisms, like floating planktonic bacteria, cluster together. When they encounter a wet surface, they stick – weakly at first but more firmly as they begin to overwhelm the area.
The bacteria proliferate to form a multi-layered microcolony and continue to grow. Once the colony reaches maturity, the bacteria secrete the protective, slimy extracellular matrix of protein and polysaccharides characteristic of biofilms. Finally, either individual or clumps of cells burst out of the biofilm and disperse, thus contaminating new surfaces.
Biofilms form anywhere at any time; they’re highly invasive, unpredictable and difficult to detect. They’re also hard to control and, once established, difficult to eliminate. This is because they’re resistant to antibiotics and disinfectants like bleach, so it’s important to be vigilant and proactive when it comes to addressing biofilm elimination.
Determining how to treat biofilms will depend on where they are. Biofilms within the body, on teeth or on dental implants, are in a sensitive part of the body and will require a different approach to those located on equipment and surfaces.
Where biofilm is found and why it poses a problem in those places
As we’ve seen, biofilms can form anytime and anywhere, but understanding each stage of biofilm formation enables you to quickly and easily eliminate them before they become established.
It’s relatively straightforward to eradicate biofilms in their early stages. Most traditional infection control products concentrate on eliminating free-floating planktonic bacteria in the first stage of growth using alcohols, quaternary ammonium compounds (QACs), chlorine-based strong acids like hypochlorite, and weaker acids like hypochlorous (HOCl).
However, eradicating biofilms in later stages of formation is far tricker, especially in human tissues whenbacteria stick to surfaces like the teeth, gums and implants, or when it accumulates in pockets in a tooth’s roots. Biofilm formation is an incredibly efficient natural process, and if left unchecked, biofilms can be extremely harmful to dental patients and lead to severe deterioration of oral health.[iv] However, conventional biofilm removal techniques, which include abrasive scraping, are often ineffective and require dentists and dental staff need to exert just the right amount of force to destroy biofilms without damaging the surrounding mucosa or implant surfaces.
Plaque, for example, can lead to oral and paranasal sinus infections, including infection or inflammation of the pulp of the tooth, or endodontic disease. Likewise, biofilms trigger gum disease or periodontitis, resulting in the characteristic loss of periodontal attachment and alveolar bone. Prostheses, dental implants and peri-implantitis infections can also be caused by biofilms and are a major cause of dental implant failure and deterioration of oral health. Biofilms located in anatomic intricacies of the root canal system are also difficult to eliminate; here irrigation is considered the primary means of cleaning and disinfecting[v] but can be tricky.
Biofilm formation is also a problem in the thin tubes of dental unit waterlines. These tubes have a narrow diameter but high surface area and are ideal breeding grounds for biofilms, particularly if left unused for long periods of time; water may stagnate in the tubes, which aids the growth of microorganisms, leading to the formation of a biofilm.[vi]
And biofilms aren’t fussy; when they disperse, they will happily relocate from instruments, worktops, devices, equipment like DUWLs, to patients and staff. This is a particular risk for severely immunocompromised patients as it can cause secondary bacterial infections.
Water from DUWLs not only enters the patient’s mouth but could come into contact with open wounds from surgical procedures or be swallowed or aspirated by patients. Vulnerable patients may be at increased risk of respiratory infection or colonisation from inhaling contaminated aerosols during dental treatment.
Tackling biofilms on or in expensive dental equipment again requires a delicate but altogether different tactic to those in organic tissues. Decontamination usually requires purging cleaning and disinfectant solutions to kill free-floating microbes followed by a shock treatment to shift established biofilms. However, a lack of clarity[vii]on the process of disinfection and maintenance of DUWLs and other areas where biofilms grow can hamper the best of intentions.
The need to be active rather than passive
The best way to assess biofilm growth is by using large and expensive scanning electron microscopes (SEM) as they provide images in high resolution and magnification,[viii] but this is well beyond the reasonable expectations of a dental professional! Therefore, it’s important focus on awareness and take practical steps to tackle biofilm formation.
Traditional biofilm treatments use a combination of mechanical interventions, abrasive scraping, and often cytotoxic chemicals (toxic to cells) to penetrate the slimy, protective extracellular matrix. These processes can feel time-consuming and arduous, but there are fast, safe (non-cytotoxic) and effective alternatives which can make the task feel less laborious.
So, what’s the ideal treatment for biofilms? It very much depends on what you’re treating – the patient or the practice. But they each require a treatment that can destroy biofilm growth at all five stages, is highly effective, quick and safe. CleanCert Hygiene, for example, have a range of products that have been independently and repeatedly proven to be highly effective against dental biofilms with short contact times and extraordinary non-toxic safety profiles.
Simon Davies is founder and Commercial Director of Tec Safe, a dental company that specialises in developing easier and safer decontamination products for a wide variety of dental applications, using eco-friendly solutions.
If you want to find out how the CleanCert Hygiene product range can proactively and reactively optimise your dental treatment outcomes, contact sales@cleancert-hygiene.co.uk or visit www.tec-safe.com today!
References
[i] Wróblewska, M., Strużycka, I., Mierzwińska-Nastalska, E. 2015. Significance of biofilms in dentistry. Przegl Epidemiol. 69(4):739-44, 879-83. Available from: https://pubmed.ncbi.nlm.nih.gov/27139354/
[ii] Woelber, JP., Al-Ahmad, A., Alt, KW. 2022. On the Pathogenicity of the Oral Biofilm: A Critical Review from a Biological, Evolutionary, and Nutritional Point of View. Nutrients 14(10):2174. Available from: https://doi.org/10.3390/nu14102174
[iii] YW., Lee, J., Lee, T-H., Lim, S. 2022. Bioelectric effect utilized a healthcare device for effective management of dental biofilms and gingivitis. Medical Engineering & Physics 104;103804. Available from: https://www.sciencedirect.com/science/article/pii/S1350453322000534?via%3Dihub
[iv] Lee, EH., Lee, S., Seo, Y., Deng, Y-H., Lim, Y-J., Kwon, H-O., Park, K., Kong, H., Kim, M-J. 2022. Manganese Oxide Nanozyme-Doped Diatom for Safe and Efficient Treatment of Peri-Implantitis. ACS Appl. Mater. Interfaces14(24): 27634–27650. Available from: https://doi.org/10.1021/acsami.2c05166
[v] Boutsioukis, C., Arias-Moliz, MT. 2022. Present status and future directions – irrigants and irrigation methods. International Endodontic Journal 55(S3):588-612. Available from: https://doi.org/10.1111/iej.13739
[vi] Umer, F., Khan, M., Khan, FR., et al. 2022. Managing dental unit waterlines: a quality improvement programme. BMJ Open Quality 11(2):e001685. Available from: https://bmjopenquality.bmj.com/content/11/2/e001685
[viii] Relucenti, M., Familiari, G., Donfrancesco, O., Taurino, M., Li, X., Chen, R., Artini, M., Papa, R., Selan, L. 2021. Microscopy Methods for Biofilm Imaging: Focus on SEM and VP-SEM Pros and Cons. Biology (Basel) 10(1):51. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7828176/
